This is quite a touchy subject for us. The main reason being, at the time our Dad was in the hospital we were not aware that he had acquired pneumonia. We were only made aware of this after the fact (once the final certificate was received)….
Please see Pneumonia (including Choking) which covers:
- Our Story
- Examples of Pneumonia on the lungs (Illustrative)
- Pneumonia
- Bilateral Bronchopneumonia
- Hospital-Acquired Pneumonia
- Aspiration Pneumonia
- Choking
- Links on Pneumonia
- Links on choking
- Our Final thoughts
© Copyright 2019 Grief Probate Journey Blog *PLEASE NOTE THIS INFORMATION IS SOURCED FROM UK and AMERICAN WEBSITES* It is also based on our own experience. *We are not experts in this field, we are speaking purely on our own experience with information sought from the internet to give further examples.*
1. Our Story
This is quite a touchy subject for us. The main reason being, at the time our Dad was in the hospital we were not aware that he had acquired pneumonia. We were only made aware of this after the fact (once the final certificate was received).
Therefore, in our case we are left looking back in hindsight about the signs we recognised, had concerns about and raised those concerns. Had we been made aware we could and would have done certain things differently and made decisions in accordance with this knowledge.
Once we learnt that our Dad had this and it was part of the cause we started doing our research, it was shocking the signs we had recognised as non-medical professionals.
Whilst putting this topic together, we have learnt so many more things that were signs we saw in our Dad.
This topic has made us realise another reason why we did this blog. When you are caring for someone 24/7 with that being your focus, you rarely have time for much else. Yes, we are saying that you need to do your research, but if someone could find all or some of the information, they need in one place that could take a little bit of the load off. At the same time, if you are not aware of what you are looking for you are not going to find it easily. Which quite often was our situation. These topics have also confirmed to us why we are pursuing our complaint with the hospital which is also a topic in this blog (Making a Complaint).
Even if you do know what you are searching for, the next thing is. Where do you start? It can be a daunting and overwhelming experience.
Another situation for us is that at the time when our Dad was in the hospital when we tried to research certain matters there wasn’t as much information readily available as there is now two years later,. Then at times, we didn’t always fully understand what we were reading, which could lead to further confusion, and so we really did struggle. Despite this, we always try and make the best of what we are facing at any particular moment in time.
We are also very aware that things are often easier said than done (researching info, continuing with daily life). Caring for someone can feel extremely pressurised, and even within everything that’s going on, you still need to find the time to take care of yourself. It’s trying to find a balance so that you can get on and get through with what you need to do. It all comes dowm to TIME (which is a topic also covered in this blog: Time: Angel Numbers: Number 7: Biblical Meaning Number 7).
This journey has been and still is a struggle. We are trying our best to make something positive come out of it, as too many of our experiences along this journey have been negative. This makes us try our best to:
- Turn Negatives into positives
- Positive Mental Attitude
This topic really makes us see why it is so important too Always speak up if:
- Something does not feel right
- Something does not look right
- Something does not sound right
- You are concerned about anything AT ALL no matter what, you must always speak up and make your concerns be heard.
- Trust your gut instinct
Our situation was complex. As our Dad had multiple medical teams we struggled to try and keep up with everything that was going on. It really was challenging times. For us during our Dads time in the hospital we often felt:
- Isolated
- Alienated
- Like we were a bother (as we were at the hospital daily)
Despite feeling this way, our main focus and concern was always our Dad’s wellbeing and care, and so we persevered and were there for him every day. He deserved nothing less than this with the illnesses he was fighting against.
Pneumonia (Including Choking): throughout the topic we use our own experiences as examples after an Internet explanation. This has been done under 7.5 and 7.6).
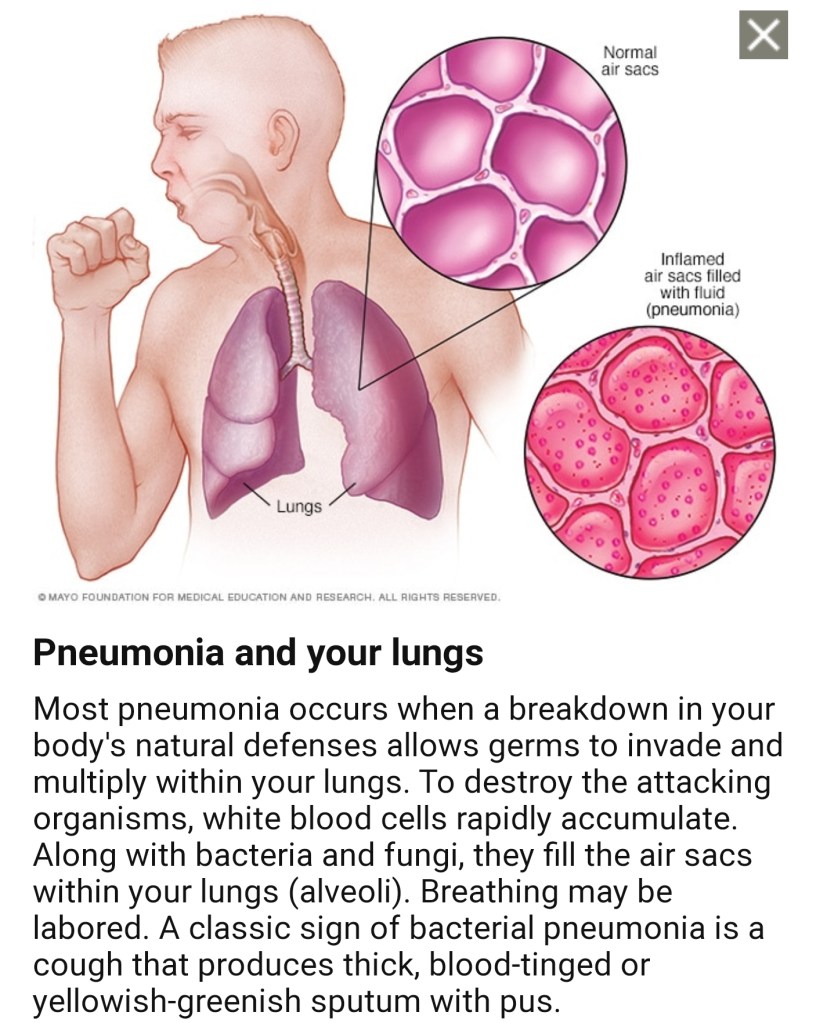
2. Examples of Pneumonia on the lungs (Illustrative)

3. Pneumonia
3.1 Pneumonia
Pneumonia is an infection that inflames the air sacs in one or both lungs. The air sacs may fill with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing. A variety of organisms, including bacteria, viruses and fungi, can cause pneumonia.
“Symptoms of pneumonia a cough – which may be dry, or produce thick yellow, green, brown or blood-stained mucus (phlegm) difficulty breathing – your breathing may be rapid and shallow, and you may feel breathless, even when resting. Chest pain – which gets worse when breathing or coughing”.
3.2 Can you catch pneumonia from someone who has it?
“Pneumonia is a lung infection caused by bacteria, viruses, or fungi. Some of these germs do spread from person to person, so you may be contagious if you have certain types of pneumonia. Fungal pneumonia passes from the environment to a person, but it’s not contagious from person to person. (18 Apr 2017)”.
3.3 How do you get pneumonia UK?
- “Community acquired pneumonia”.
- “Community acquired is when a person who has little contact with the healthcare system contracts the condition”.
- “The most common cause of pneumonia is a pneumococcal infection, caused by bacteria called Streptococcus pneumoniae”.
- “In the UK, pneumonia affects around 1 in 1000 adults each year”.
3.4 Which type of pneumonia is the most serious?
“The main types of pneumonia are: Bacterial pneumonia. This type is caused by various bacteria. The most common is Streptococcus pneumoniae”.
What are the danger signs of pneumonia?
The signs and symptoms of pneumonia may include:
- “Cough, which may produce greenish, yellow or even bloody mucus”.
- “Fever, sweating and shaking chills”.
- “Shortness of breath”.
- “Rapid, shallow breathing”.
- “Sharp or stabbing chest pain that gets worse when you breathe deeply or cough”.
- “Loss of appetite, low energy, and fatigue”.
More items… (31 Dec 2018).
3.5 Do you have a temperature with pneumonia?
“The symptoms of bacterial pneumonia can develop gradually or suddenly. Fever may rise as high as a dangerous 105 degrees F, with profuse sweating and rapidly increased breathing and pulse rate. Early symptoms are similar to influenza symptoms: fever, a dry cough, headache, muscle pain, and weakness. (31 Dec 2018)”.
3.6 Is Cold air bad for pneumonia?
“Cooler air can, however, exacerbate an existing cough. So if you have a cold or other respiratory infection – such as pneumonia or bronchitis – then being outside in the cold can make you cough. This is why most coughs seem to get worse when the temperature falls after dark. (24 Jul 2012)”
3.7 Can lungs repair themselves after pneumonia?
“Living With Pneumonia”
“Amazingly, even with severe pneumonia, the lung usually recovers and has no lasting damage, although occasionally there might be some scarring of the lung (rarely leading to bronchiectasis) or lung surface (the pleura)”.
3.8 What causes pneumonia in hospital patients?
“Hospital-acquired pneumonia is most commonly caused by the following bacteria: Streptococcus pneumoniae. Staphylococcus aureus (including methicillin-resistant Staphylococcus aureus [MRSA]) Gram-negative bacteria such as Pseudomonas aeruginosa and Haemophilus influenzae”.
Why do hospital patients get pneumonia?
“People in hospitals and retirement homes are often older, bedridden or weakened as a result of disease or surgery. That is why they more frequently develop severe pneumonia with complications. That risk is particularly high in patients who become infected with pneumonia while receiving artificial respiration. (25 Jul 2018)”.
How long do you stay in the hospital for pneumonia?
“4 to 6 days”
“The average amount of time to stay in the hospital to treat pneumonia is 4 to 6 days. Your provider will make sure that you are breathing easily, your oxygen levels and other medical conditions are stable, and that you will be able to care for yourself when you go home”.
How do hospitals prevent pneumonia?
“Traditional preventive measures for nosocomial pneumonia include decreasing aspiration by the patient, preventing cross-contamination or colonization via hands of personnel, appropriate disinfection or sterilization of respiratory-therapy devices, use of available vaccines to protect against particular infections, and. (3 Jan 1997)”.
3.9 What are the chances of surviving pneumonia?
“Pneumonia can also be fatal. The mortality (death) rate is up to 30% for patients with severe pneumonia who require treatment in an intensive care unit. Overall, around 5%-10% of patients who are treated in a hospital setting die from the disease”.
What is the fastest way to cure pneumonia?
“How Is Pneumonia Treated?”
- “Control your fever with aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs, such as ibuprofen or naproxen), or acetaminophen.”
- “Drink plenty of fluids to help loosen secretions and bring up phlegm”.
- “Do not take cough medicines without first talking to your doctor.”
More items… (31 Dec 2018)
3.9.1 How do I know if I am over pneumonia?
“Mild signs and symptoms often are similar to those of a cold or flu, but they last longer. Signs and symptoms of pneumonia may include: Chest pain when you breathe or cough. Confusion or changes in mental awareness (in adults age 65 and older)”.
3.9.2 How long does fatigue last after pneumonia?
“Ninety days after diagnosis, 51 percent reported fatigue, 32 percent cough, and 28 percent shortness of breath. Another study surveyed 500 pneumonia patients age 50 and older and found that tiredness, weakness and shortness of breath lasted more than three weeks, on average (2 Jan 2017)”.
3.9.3 Can Pneumonia cause sudden death?
“Pneumonia is the leading infectious cause of death. Early deterioration and death commonly result from progressive sepsis, shock, respiratory failure, and cardiac complications. Recent data suggest that cardiac arrest may also be common, yet few previous studies have addressed this. (22 Dec 2011”).
4. Bilateral Bronchopneumonia
4.1 What is bilateral bronchopneumonia?
“Bronchopneumonia is a type of pneumonia, a condition that causes inflammation of the lungs. Symptoms can range from mild to severe and may include coughing, breathing difficulties, and fever. Causes include bacterial, viral, or fungal chest infections. (25 Sep 2018)”
4.2 Bilateral Bronchopneumonia
“It occurs when viruses, bacteria, or fungi cause inflammation and infection in the alveoli (tiny air sacs) in the lungs. Bronchopneumonia is a type of pneumonia that causes inflammation in the alveoli. Someone with bronchopneumonia may have trouble breathing because their airways are constricted. (19 Apr 2019)”.
4.3 Is bronchopneumonia contagious?
“Many cases of bronchopneumonia are caused by bacteria. Outside the body, the bacteria are contagious and can spread between people in close proximity through sneezes and coughs. A person becomes infected by breathing in the bacteria”.
4.4 What is the difference between pneumonia and bronchopneumonia?
“What is the difference between bronchopneumonia and lobar pneumonia? Bronchopneumonia: Characterized by patchy foci of consolidation (pus in many alveoli and adjacent air passages) scattered in one or more lobes of one or both lungs. Lobar pneumonia: Characterized by an acute inflammation of the entire lobe or lung.”
4.5 How serious is bronchial pneumonia?
“Chronic bronchitis”.
“Pneumonia is another infection in your lungs, but instead of the bronchial tubes, you get it in tiny air sacs in your lungs called alveoli. It can be mild, but sometimes serious, especially for the very young, adults 65 or older, and people with weaker immune systems. (23 Dec 2018)”.
4.6 How do you prevent bronchopneumonia?
Besides getting shots, you can lower your risk of getting bacterial pneumonia by doing these things:
- “Wash your hands regularly, especially after you go to the bathroom and before you eat”.
- “Eat right, with plenty of fruits and vegetables”.
- “Exercise”.
- “Get enough sleep”.
- “Quit smoking”.
- “Stay away from sick people, if possible”. (23 Nov 2018)
5. Hospital-Acquired Pneumonia
5.1 Hospital-Acquired Pneumonia
“What is hospital induced pneumonia?”
“Hospital–acquired pneumonia (HAP) is an acute lower respiratory tract infection that is by definition acquired after at least 48 hours of admission to hospital and is not incubating at the time of admission”.
5.2 What is hospital acquired pneumonia NHS?
“Hospital Acquired Pneumonia (HAP) is defined as pneumonia that occurs 48 hours or more after admission to hospital”.
5.3 How do patients get hospital acquired pneumonia?
“Hospital–acquired pneumonia can also be spread by health care workers, who can pass germs from their hands or clothes from one person to another. People can be more likely to get pneumonia while in the hospital if they: Abuse alcohol. Have had chest surgery or other major surgery. (16 Jul 2017)”.
5.4 How is hospital acquired pneumonia treated?
“In general, for both hospital–acquired pneumonia (HAP) and VAP, 7 days of treatment with appropriate antibiotics/antibiotics is recommended. (30 Jul 2018)”.
5.5 What can help prevent hospital acquired pneumonia?
“Traditional preventive measures for nosocomial pneumonia include decreasing aspiration by the patient, preventing cross-contamination or colonization via hands of HCWs, appropriate disinfection or sterilization of respiratory-therapy devices, use of available vaccines to protect against particular infections. (3 Jan 1997).”
5.6 What is the most common cause of hospital acquired pneumonia?
“Hospital–acquired pneumonia (HAP) develops at least 48 hours after hospital admission. The most common pathogens are gram-negative bacilli and Staphylococcus aureus; antibiotic-resistant organisms are an important concern”.
5.7 Can you die from hospital acquired pneumonia?
“Prognosis. Despite receiving excellent treatment, a high percentage of people who develop hospital–acquired pneumonia die. However, death is often related to the underlying health problems that allowed the pneumonia to develop (for example, widespread cancer)”
6. Aspiration Pneumonia
6.1 Can aspiration pneumonia be cured?
“Aspiration pneumonia is a lung infection caused by inhaled oral or gastric contents. It can become serious if left untreated. Treatment involves antibiotics and supportive care for breathing. Most people (79 percent) will survive aspiration pneumonia”.
6.2 How can you tell if someone aspirated?
What are the symptoms of aspiration from dysphagia?
- “Feeling that food is sticking in your throat or coming back into your mouth”.
- “Pain when swallowing”.
- “Trouble starting a swallow”.
- “Coughing or wheezing after eating”.
- “Coughing while drinking liquids or eating solids”.
- “Chest discomfort or heartburn”.
What are the symptoms of aspiration pneumonia?
- “Chest pain”.
- “Shortness of breath”.
- “Wheezing”.
- “Fatigue”.
- “Blue discoloration of the skin”.
- “Cough, possibly with green sputum, blood, or a foul odor”.
- “Difficulty swallowing”.
- “Bad breath”.
How long after aspiration do symptoms occur?
“Patients often have a latent period after the aspiration event and the onset of symptoms. Symptoms usually occur within the first hour of aspiration, but almost all patients have symptoms within 2 hours of aspiration. (19 May 2017)”.
6.3 How long does it take to recover from aspiration pneumonia?
“1 to 4 weeks”
“The tube will be removed when the drainage stops and your chest X-ray shows improvement. With treatment, you may recover in 1 to 4 weeks. If you are over 60 years old or have other medical problems, it may take longer to get your strength back and feel normal”.
6.4 What part of the lung is affected by aspiration pneumonia?
“Radiographic evidence of aspiration pneumonia depends on the position of the patient when the aspiration occurred. The right lower lung lobe is the most common site of infiltrate formation due to the larger caliber and more vertical orientation of the right mainstem bronchus. (15 Aug 2018)”.
What lobe is affected in aspiration pneumonia?
“The usual site for an aspiration pneumonia is the apical and posterior segments of the lower lobe of the right lung. If the patient is supine then the aspirated material may also enter the posterior segment of the upper lobes.(30 Nov 2016)”,
6.5 Can a feeding tube cause aspiration pneumonia?
“Aspiration. Aspiration is one of the most important and controversial complications in patients receiving enteral nutrition, and is among the leading causes of death in tube–fed patients due to aspiration pneumonia. … The rate of aspiration pneumonia in tube–fed patients ranges from approximately 5% to 58%”.
6.6 Does aspiration always lead to pneumonia?
“Aspiration can cause lung inflammation (chemical pneumonitis), infection (bacterial pneumonia or lung abscess), or airway obstruction. However, most episodes of aspiration cause minor symptoms or pneumonitis rather than infection or obstruction, and some patients aspirate with no sequelae”.
6.7 What does aspiration pneumonia feel like?
“A high fever and difficulty breathing may indicate aspiration pneumonia. Aspiration pneumonia can cause a range of symptoms, including: difficulty swallowing. shortness of breath or difficulty breathing. (8 Jun 2018)”.
6.8 What are signs of silent aspiration?
“Silent aspiration usually has no symptoms, and people aren’t aware that fluids or stomach contents have entered their lungs. Overt aspiration will usually cause sudden, noticeable symptoms such as coughing, wheezing, or a hoarse voice. Silent aspiration tends to occur in people with impaired senses”.
6.9 Can Aspiration Pneumonia cause Sepsis?
“The two most common infections that cause sepsis are urinary, as from a urinary tract infection, or respiratory, as from pneumonia. For example, someone who has difficulty swallowing may aspirate food or drink (get food or drink into their airway) and can develop aspiration pneumonia”. (10 Mar 2019).
6.9.1 How can you prevent aspiration with dysphagia?
“PREVENTION OF ASPIRATION DURING HAND FEEDING”:
- “Sit the person upright in a chair; if confined to bed, elevate the backrest to a 90-degree angle”.
- “Implement postural changes that improve swallowing”.
- “Adjust rate of feeding and size of bites to the person’s tolerance; avoid rushed or forced feeding”
6.9.2 How do you prevent aspiration pneumonia?
“To reduce the risk of aspiration pneumonia, maintenance of good oral hygiene is important and medications affecting salivary flow or causing sedation are best avoided, if possible. The use of H2 blockers and proton-pump inhibitors should be minimised. (4 Jul 2014)”.
6.9.3 Is silent aspiration dangerous?
“Swallowing problems can lead to aspiration. Aspiration describes a condition when food or fluids that should go into the stomach go into the lungs instead. This is known as a “silent aspiration.” Frequent aspiration can cause damage to the lungs if it is not treated”.
6.9.4 Can poor oral care lead to aspiration pneumonia?pl
“This can lead to aspiration pneumonia, and, subsequently, an increased risk of hospital transfers, morbidity, and mortality. Key words: Aspiration, aspiration pneumonia, aspiration prevention, dysphagia, lower respiratory tract infections, medication use, oral hygiene”.
6.9.5 What happens when you die from aspiration pneumonia?
“While pneumonia is a serious infection, it has a relatively low mortality. The condition that caused aspiration, combined with the increased potential for sepsis, raises the risk of serious complication or death. (1 Jan 2009)”.
6.9.6 How does aspiration cause death?
“Death from Aspiration Pneumonia. Aspiration occurs when foreign material is inhaled into the airway. Causes of death include asphyxiation due to a blocked airway and irritation or infection of the respiratory tract due to inhaled material, or aspiration pneumonia, which will be the primary focus of this segment”.
7. Choking
7.1 Choking
“Choking occurs when an object becomes stuck in the throat or the windpipe and blocks air from flowing into the lungs. In some cases the air flow is completely blocked, in other cases some amount of air can pass to the lungs”.
“Choking (also known as foreign body airway obstruction) is a life-threatening medical emergency characterized by the blockage of air passage into the lungs secondary to the inhalation or ingestion of food or another object. Choking is caused by a mechanical obstruction of the airway that prevents normal breathing”.
7.3 “What are signs and symptoms of choking?”
“The danger signs of choking are”:
- “Bluish skin color”.
- “Difficulty breathing — ribs and chest pull inward”.
- “Loss of consciousness (unresponsiveness) if blockage is not cleared”.
- “Inability to cry or make much sound”.
- “Weak, ineffective coughing”.
- “Soft or high-pitched sounds while inhaling”. (12 Jan 2019).
7.4 Does choking happen immediately?
“Choking can cause a simple coughing fit, but complete blockage of the airway may lead to death. Choking is a true medical emergency that requires fast, appropriate action by anyone available. Emergency medical teams may not arrive in time to save a choking person’s life. Breathing is an essential part of life”.
7.5 “What are the risks of choking?”
“Factors that Increase the Risk of Choking”
- “Neurological and muscular disorders such as cerebral palsy and seizure disorders”.
- “Dysphagia (difficulty swallowing)”
- “Side effects from medications”.
- “Gastroesphogeal reflux disease (GERD)”
- “Difficulty swallowing”.
- “Few or no teeth”.
- “Dentures”.
In our case, our Dad had developed a poor swallow during his time in the hospital. This resulted in him being referred to the SALT Team – Speech and Language Therapy Team. This also meant that our Dads diet had to be modified due to the change in his condition.
7.6 Universal Signs of Choking
“The universal sign for choking is when a person puts his clutched hands on the throat. Other signs and symptoms include the inability to talk, coughing, wheezing, gagging, squeaky sounds when trying to breathe, difficulty in breathing, pale or bluish color of the skin and loss of consciousness”.
I was witness to our Dad choking. It was such a surreal scary and traumatic experience. I didn’t realise that my Dad was choking, to begin with as I had taken my eye off of him for a second, and it was silent, when I turned back around that is when I realised as, his lips had started turning blue, he was grabbing the sheets on the bed, it was such a horrible thing to see. I knew this was serious and that I needed help, and so I ran out of the room and found someone in the ward to help me.
What happened next was a feeling out of this world. The person that came to help assessed my Dad could see it was a serious matter, and so they pressed a button in the room (I think a red button) I was outside of the room at this time to give them space to do what was needed. Once that button was pressed, out of every room, all the hospital staff appeared that were on the ward at the time and ran into my Dad’s room. I literally felt like I was on the set of a movie, but this was my current situation, it was really real and really happening.
Thankfully with the actions taken, our Dad made good recovery. But it was very touch and go. One minute I was being told that he might not make it through the night, and the next I was talking to him and helping him to spit once he’d cleared his throat. It was such a scary experience, I felt very strange being in the room with him on my own so soon after it happened for the fear that it could happen again. It was also very surreal for me. I hadn’t even had the time to compose myself and process what had happened, and so being left on my own with our Dad was quite scary. The only reason why I felt more comfortable is because I could see our Dad had recovered from the incident, and was starting to come back to himself
After that time I didn’t feel comfortable feeding him anymore, again for the fear it could happen.
I have never experienced something like that in my life, and I hope I never do again. I was just grateful that my Dad made it through, I do not know how I would have coped if it had gone any other way.
The thing about it is, I’m saying how scary the experience was for me, we can’t even begin to image what it must have been like/felt like for our Dad. This incident made him extremely cautious about wanting to eat again. The pain and suffering he endured during the time he was in the hospital, we feel sadness about it evey single day.
7.7 What causes choking in elderly?
“Some common causes: Teeth in bad condition or poorly fitting dentures. Normal aging (weakening of mouth/throat muscles) Acid reflux (GERD)”.
As previously mentioned in our topic on Infective Endocarditis, our Dad had issues with his gums. He didn’t have many teeth and so required dentures. The dentures that were made for him never fitted accurately despite numerous moulds being made for him. He visited the dentist and hospital regularly because of these reasons.
7.8 How common is choking to death
“Thousands of People Die From Choking Every Year
According to Injury Facts 2017, choking is the fourth leading cause of unintentional injury death. Of the 5,051 people who died from choking in 2015, 2,848 were older than 74”.
How long does it take to die from choking?
“The lack of oxygen caused by choking can result in brain damage or death in four to six minutes”.
7.9 How can you prevent choking?
These tips will also help reduce incidences of choking:
- “Don’t drink fluids while you’re eating”.
- “Don’t talk while you eat”.
- “Don’t eat lying down”.
- “Don’t drink alcohol while eating”.
- “Do learn to eat more slowly”.
- “Do put less on your plate so you can’t eat too much too fast.”
- “Do julienne the food”.
8. Links on Pneumonia
8.1 Pneumonia
- Pneumonia Treatment – NHS
- Pneumonia British Lung Foundation
- Symptoms of Pneumonia British Lung Foundation
- Pneumonia Health Information – BUPA UK
- Pneumonia Patient Information – University Hospital
- What is Pneumonia? Symptoms – Causes – Treatments
- Pneumonia in Adults – NICE
8.2 Hosptial Acquired Pneumonia
- Hospital Acquired Pneumonia General Practice Notebook
- Guidelines for the Management of Hospital Acquired Pneumonia
8.3 Aspiration Pneumonia
- Aspiration Pneumonia Pathway
- Aspiration Pneumonia – Symptoms and Treatment
- Aspiration Pneumonia. What are the common causes?
9. Links on Choking:
- https://www.nhs.uk/common-health-questions/accidents-first-aid-and-treatments/what-should-i-do-if-someone-is-choking/
- https://www.mayoclinic.org/first-aid/first-aid-choking/basics/art-20056637
- https://www.nidirect.gov.uk/conditions/blue-skin-and-lips-cyanosis
- https://www.nhs.uk/conditions/blue-skin-or-lips-cyanosis/
10. Our final thoughts
This blog is turning out to be a learning experience for us. Which we are not quite sure we expected to happen.
We are actually learning more as we source information to provide. It is opening up our eyes to our Dads medical conditions and how much they were interlinked and so closely related. At the time it was so hard to see as we were in the moment of that time. And at that time so many complex things were occurring that it was so difficult to be able to process information from one instance to the next.
Over two years after our Dad passing, we are still finding out more and more information that we were not aware of. It is mindblowing and very strange to digest. We feel this is because we have pushed aside those times in order to be able to handle the probate process.
All along we have said we knew that once things started to slow down is when things would become more real, but this is different, we are learning more things and so it is becoming real in ways that we wouldn’t have imagined.
I guess our final thoughts would be, if in a situation where you are caring for someone with multiple medical conditions, the best and only thing you can do, is your best. And also try to not beat yourself up too much if you start to feel as though your best is not good enough. In any situation, you are only one person, and there is only so much that you can do. Also what needs to be remembered is that you are not the medical professional, so again, you are limited to what you can do.
We would also advise to gain as much knowledge as possible so that you are mentally prepared as possible for what you are facing.
One thought on “Pneumonia (Including Choking)”